UG Krishnamurti
Member
- Joined
- Sep 28, 2020
- Messages
- 555
RP: " Among the factors that probably have a role in preventing cataracts: Thyroid, progesterone, pregnenolone, vitamin E, iodide, pyruvate. Increasing the carbon dioxide lowers the cell’s pH, and tends to resist swelling. Palmitic acid (a saturated fat that can be synthesized by our tissues) is normally oxidized by the lens. Calcium blockers experimentally prevent cataracts, suggesting that magnesium and thyroid (which also act to exclude calcium from cells) would have the same effect."
RP: [ IODIDE ]: The sea cucumber has been used to study the physical properties of connective tissue, and it has been found that certain salts tend to soften the connective tissues, but that iodide doesn't. The well-established use of iodide to resolve granulomas, even when it doesn't eliminate the infectious agent, might suggest that it is protecting against something which is disrupting the connective tissue structure. The only publications I have seen that presented clear evidence of the disappearance of arteriosclerosis involved treatment with iodides. In the retina, blood vessels can be seen to return to their normal appearance following a course of iodide treatment. Besides its possible direct effects on the mucins, iodide might help to eliminate calcium from the walls of blood vessels, since calcium iodide is very soluble.
RP: Besides its possible direct effects on the mucins, iodide might help to eliminate calcium from the walls of blood vessels, since calcium iodide is very soluble.
RP: Endotoxin, produced by bacteria, mainly in the intestine, disrupts energy production, and promotes maladaptive inflammation. The wide spectrum of benefit that iodide has, especially in diseases with an inflammatory component, suggests first that it protects tissue by blocking free radical damage, but it also suggests the possibility that it might specifically protect against endotoxin.
RP: One of the best-known free radical scavenging substances that has been widely used as a drug is iodide. It has been used to treat asthma, parasites, syphilis, cancer, Graves’ disease, periodontal disease, and arteriosclerosis. Diseases that produce tissue overgrowth associated with inflammation--granulomas--have been treated with iodides, and although the iodide doesn’t necessarily kill the germ, it does help to break down and remove the granuloma. Leprosy and syphilis were among the diseases involving granulomas* that were treated in this way. In the case of tuberculosis, it has been suggested that iodides combine with unsaturated fatty acids which inhibit proteolytic enzymes, and thus allow for the removal of the abnormal tissue.
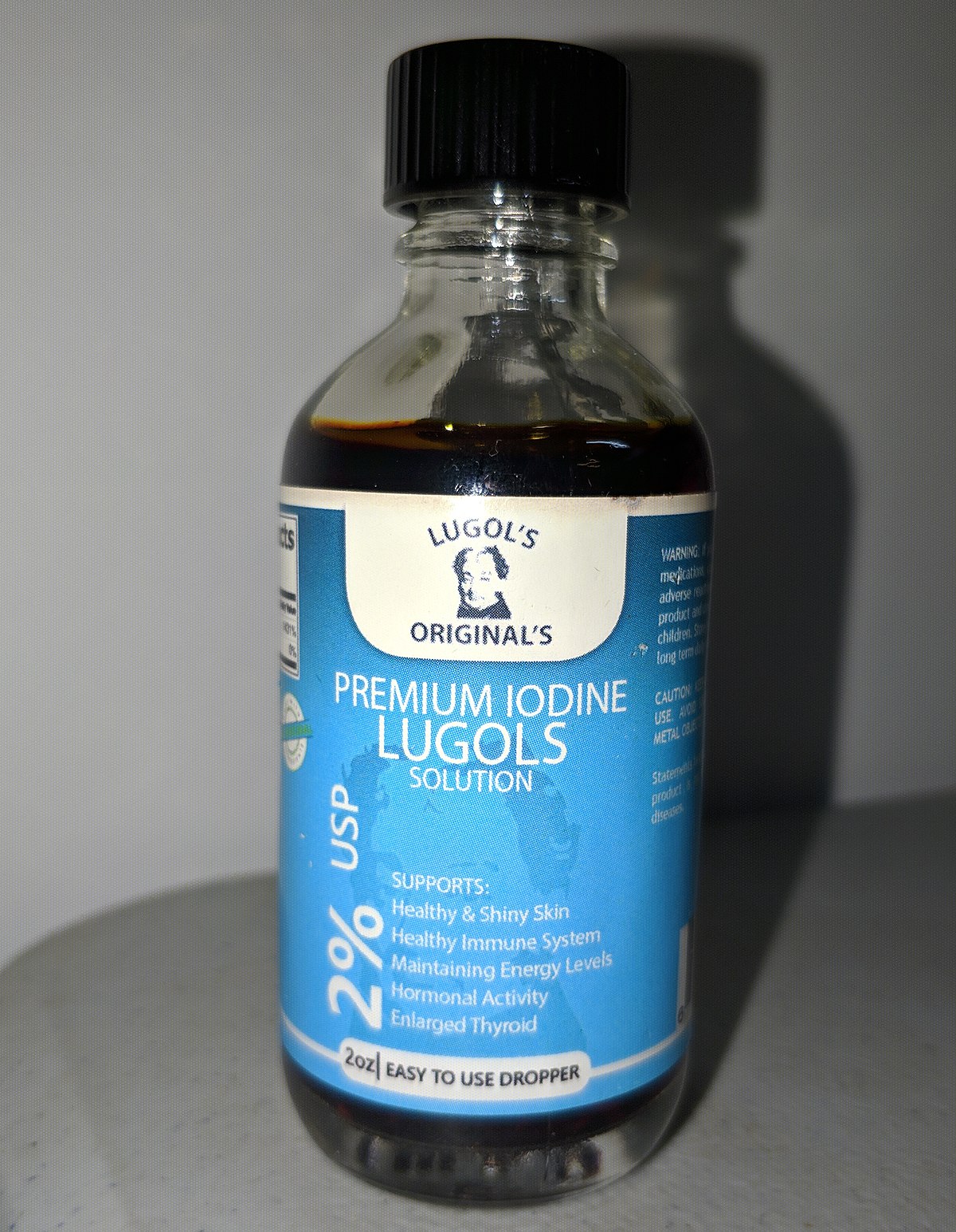
Did anyone had experiences with iodide and how and where should one get iodide from?
@Hans @haidut Do you have any info? Much love guys.
RP: [ IODIDE ]: The sea cucumber has been used to study the physical properties of connective tissue, and it has been found that certain salts tend to soften the connective tissues, but that iodide doesn't. The well-established use of iodide to resolve granulomas, even when it doesn't eliminate the infectious agent, might suggest that it is protecting against something which is disrupting the connective tissue structure. The only publications I have seen that presented clear evidence of the disappearance of arteriosclerosis involved treatment with iodides. In the retina, blood vessels can be seen to return to their normal appearance following a course of iodide treatment. Besides its possible direct effects on the mucins, iodide might help to eliminate calcium from the walls of blood vessels, since calcium iodide is very soluble.
RP: Besides its possible direct effects on the mucins, iodide might help to eliminate calcium from the walls of blood vessels, since calcium iodide is very soluble.
RP: Endotoxin, produced by bacteria, mainly in the intestine, disrupts energy production, and promotes maladaptive inflammation. The wide spectrum of benefit that iodide has, especially in diseases with an inflammatory component, suggests first that it protects tissue by blocking free radical damage, but it also suggests the possibility that it might specifically protect against endotoxin.
RP: One of the best-known free radical scavenging substances that has been widely used as a drug is iodide. It has been used to treat asthma, parasites, syphilis, cancer, Graves’ disease, periodontal disease, and arteriosclerosis. Diseases that produce tissue overgrowth associated with inflammation--granulomas--have been treated with iodides, and although the iodide doesn’t necessarily kill the germ, it does help to break down and remove the granuloma. Leprosy and syphilis were among the diseases involving granulomas* that were treated in this way. In the case of tuberculosis, it has been suggested that iodides combine with unsaturated fatty acids which inhibit proteolytic enzymes, and thus allow for the removal of the abnormal tissue.
Did anyone had experiences with iodide and how and where should one get iodide from?
@Hans @haidut Do you have any info? Much love guys.