OP
TreasureVibe
Member
- Joined
- Jul 3, 2016
- Messages
- 1,941
Haidut adviced keto-acids for advanced cancer:
Keto acid - Wikipedia
Keto acids or ketoacids (also called oxo acids or oxoacids) are organic compounds that contain a carboxylic acid group and a ketone group.[1] In several cases, the keto group is hydrated. The alpha-keto acids are especially important in biology as they are involved in the Krebs citric acid cycle and in glycolysis.[2]
Common types of keto acids include:
When ingested sugars and carbohydrate levels are low, stored fats and proteins are the primary source of energy production. Glucogenic amino acids from proteins are converted to glucose. Ketogenic amino acids can be deaminated to produce alpha keto acids and ketone bodies.
Alpha keto acids are used primarily as energy for liver cells and in fatty acid synthesis, also in the liver.
Maybe either Oxaloacetic acid - Wikipedia or Acetoacetic acid - Wikipedia are good for cancer?
Acetoacetic acid (also diacetic acid) is the organic compound with the formula CH3COCH2COOH. It is the simplest beta-keto acid group, and like other members of this class, it is unstable. The methyl and ethyl esters, which are quite stable, are produced on a large scale industrially as precursors to dyes. Acetoacetic acid is a weak acid.[3]
Biochemistry
Under typical physiological conditions, acetoacetic acid exists as its conjugate base, acetoacetate.
Acetoacetate is produced in mitochondria of the liver from acetoacetyl Coenzyme A (CoA). First another acetyl group is added from acetyl CoA to form 3-hydroxy-3-methylgluteryl CoA, and then an acetyl CoA is lost from this yielding acetoacetate. The initial acetoacetate can come from the last cycle in the beta oxidation of a fatty acid, or it can be synthesized from two acetyl CoA molecules, catalyzed by thiolase.[4]
In mammals acetoacetate produced in the liver (along with the other two "ketone bodies") is released into the bloodstream as an energy source during periods of fasting, exercise, or as a result of type 1 diabetes mellitus.[5] First a CoA group is enzymatically transferred to it from succinyl CoA, converting it back to acetoacetyl CoA. This is then broken into two acetyl CoA molecules by thiolase, and these then enter the citric acid cycle. Heart muscle and renal cortex prefer acetoacetate over glucose. The brain uses acetoacetate when glucose levels are low due to fasting or diabetes.[6]
Acetoacetic acid - Wikipedia
Oxaloacetic acid (also known as oxalacetic acid) is a crystalline organic compound with the chemical formula HO2CC(O)CH2CO2H. Oxaloacetic acid, in the form of its conjugate base oxaloacetate, is a metabolic intermediate in many processes that occur in animals. It takes part in the gluconeogenesis, urea cycle, glyoxylate cycle, amino acid synthesis, fatty acid synthesis and citric acid cycle.[1]
Biosynthesis[edit]
Oxaloacetate forms in several ways in nature. A principal route is upon oxidation of L-malate, catalysed by malate dehydrogenase, in the citric acid cycle. Malate is also oxidized by succinate dehydrogenase in a slow reaction with the initial product being enol-oxaloacetate.[2]
It also arises from the condensation of pyruvate with carbonic acid, driven by the hydrolysis of ATP:
CH3C(O)CO2− + HCO3− + ATP → −O2CCH2C(O)CO2− + ADP + Pi
Occurring in the mesophyll of plants, this process proceeds via phosphoenolpyruvate, catalysed by pyruvate carboxylase.
Oxaloacetate can also arise from trans- or de- amination of aspartic acid.
Biochemical functions[edit]
Oxaloacetate is an intermediate of the citric acid cycle, where it reacts with acetyl-CoA to form citrate, catalysed by citrate synthase. It is also involved in gluconeogenesis, urea cycle, glyoxylate cycle, amino acid synthesis, and fatty acid synthesis. Oxaloacetate is also a potent inhibitor of Complex II.
Gluconeogenesis[edit]
Gluconeogenesis[1] is a metabolic pathway consisting of a series of eleven enzyme-catalyzed reactions, resulting in the generation of glucose from non-carbohydrates substrates. The beginning of this process takes place in the mitochondrial matrix, where pyruvate molecules are found. A pyruvate molecule is carboxylated by a pyruvate carboxylase enzyme, activated by a molecule each of ATP and water. This reaction results in the formation of oxaloacetate. NADH reduces oxaloacetate to malate. This transformation is needed to transport the molecule out of the mitochondria. Once in the cytosol, malate is oxidized to oxaloacetate again using NAD+. Then oxaloacetate remains in the cytosol, where the rest of reactions will take place. Oxaloacetate is later decarboxylated and phosphorylated by phosphoenolpyruvate carboxykinase and becomes 2-phosphoenolpyruvate using guanosine triphosphate (GTP) as phosphate source. Glucose is obtained after further downstream processing.
Urea cycle[edit]
The urea cycle is a metabolic pathway that results in the formation of urea using two ammonium molecules and one bicarbonate molecule.[1] This route commonly occurs in hepatocytes. The reactions related to the urea cycle produce NADH), and NADH can be produced in two different ways. One of these uses oxaloacetate. In the cytosol there are fumarate molecules. Fumarate can be transformed into malate by the actions of the enzyme fumarase. Malate is acted on by malate dehydrogenase to become oxaloacetate, producing a molecule of NADH. After that, oxaloacetate will be recycled to aspartate, as transaminases prefer these keto acids over the others. This recycling maintains the flow of nitrogen into the cell.
Glyoxylate cycle[edit]
The glyoxylate cycle is a variant of the citric acid cycle.[3] It is an anabolic pathway occurring in plants and bacteria utilizing the enzymes isocitrate lyase and malate synthase. Some intermediate steps of the cycle are slightly different from the citric acid cycle; nevertheless oxaloacetate has the same function in both processes.[1] This means that oxaloacetate in this cycle also acts as the primary reactant and final product. In fact the oxaloacetate is a net product of the glyoxylate cycle because its loop of the cycle incorporates two molecules of acetyl-CoA.
Fatty acid synthesis[edit]
In previous stages acetyl-CoA is transferred from the mitochondria to the cytoplasm where fatty acid synthase resides. The acetyl-CoA is transported as a citrate, which has been previously formed in the mitochondrial matrix from acetyl-coA and oxaloacetate. This reaction usually initiates the citric acid cycle, but when there is no need of energy it is transported to the cytoplasm where it is broken down to cytoplasmatic acetyl -CoA and oxaloacetate.
Another part of the cycle requires NADPH for the synthesis of fatty acids.[4] Part of this reducing power is generated when the cytosolic oxaloacetate is returned to the mitochondria as long as the internal mitochondrial layer is non-permeable for oxaloacetate. Firstly the oxaloacetate is reduced to malate using NADH. Then the malate is decarboxylated to pyruvate. Now this pyruvate can easily enter the mitochondria, where it is carboxylated again to oxaloacetate by pyruvate carboxylase. In this way, the transfer of acetyl-CoA that is from the mitochondria to the outside of the cell into the cytoplasm produces a molecule of NADH. The overall reaction, which is spontaneous, may be summarized as:
HCO3− + ATP + acetyl-CoA → ADP + Pi + malonyl-CoA
Amino acid synthesis[edit]
Six essential amino acids and three nonessential are synthesized from oxaloacetate and pyruvate.[5] Aspartate and alanine are formed from oxaloacetate and pyruvate, respectively, by transamination from glutamate. Asparagine, methionine, lysine and threonine are synthesized by aspartate, therefore given importance to oxaloacetate as without it, no aspartate would be formed and the following other amino acids would neither be produced.
Oxalate biosynthesis[edit]
Oxaloacetate produces oxalate by hydrolysis.[6]
oxaloacetate + H2O ⇌ oxalate + acetate
This process is catalyzed by the enzyme oxaloacetase.
Oxaloacetic acid - Wikipedia
Found this:
Acetoacetate is a metabolic inhibitor of cancer growth
Acetoacetate reduces growth and ATP concentration in cancer cell lines which over-express uncoupling protein 2. - PubMed - NCBI
Acetoacetate reduces growth and ATP concentration in cancer cell lines which over-express uncoupling protein 2
Addicted to AA (Acetoacetate): A Point of Convergence between Metabolism and BRAF Signaling
Prevention of Dietary-Fat-Fueled Ketogenesis Attenuates BRAF V600E Tumor Growth - ScienceDirect
Acetoacetate metabolism in AS-30D hepatoma cells
New Study Found Oxaloacetate Could Fight Cancer and Give Calorie Restriction Benefits
The metabolic fate of acetate in cancer
8) Oxaloacetate May Help Cancer
Glutamine is an important growth element for pancreatic cancer cells [R].
Studies have shown that reducing glutamine levels can stop cell growth of multiple forms of cancer [R].
Oxaloacetate has been shown to reduce glutamine levels and decrease cancer cell growth rates in mice [R].
It has also been shown to make chemotherapy and radiation treatment more effective [R].
Source: 15 Science-Based Health Benefits of Oxaloacetate - Selfhacked
Glutamine Addiction: A New Therapeutic Target in Cancer
Oxaloacetate induces apoptosis in HepG2 cells via inhibition of glycolysis
Oxaloacetate: 3 Outrageous Reasons This Molecule... - Nootropedia
Oxaloacetate: The Next Big Brain & Anti-Aging Supplement?
3 Ways an Oxaloacetate Supplement Can Protect You
CRONaxel is a US FDA registered combination of oxaloacetate and ascorbic acid for the clinical dietary management of the metabolic imbalances associated with certain cancers. (Oxaloacetate has the designation as an “orphan drug 12-3704” for the treatment of neuro-endocrine and glial tumors.)
Oxaloacetate is an obscure molecule that plays a role in energy production. Researchers have learned that it can also remove excess glutamate from the bloodstream. Glutamate can cause extensive brain damage in the event of a stroke or concussion, and it is a preferred fuel for many different types of cancer cells. Oxaloacetate’s removal of glutamate has a protective effect against these hazards.
Oxaloacetate increases energy production:
Cells can produce energy in two different ways. The more primitive, less effective method is glycolysis. The more advanced and efficient method is oxidative phosphorylation. This occurs in the mitochondria, and it produces eight times more energy than glycolysis—while using the same amount of fuel.[1] Oxaloacetate is an important part of the metabolic cycle that allows oxidative phosphorylation to occur. Without this molecule, cells are forced to rely more heavily on glycolysis.[2] This can lead to decreased production of energy and a decreased supply of blood sugar. In fact, studies indicate that a lack of oxaloacetate can cause energy production to fall by nearly 500%.[3]
Oxaloacetate starves cancer:
Cancerous cells rely on simple sugars and glutamate for their fuel supply, and this is especially true for brain tumors.[4] Glutamate also allows cancer cells to grow and divide.[5] When simple sugars and glutamate are abundant, cancer cells can produce more energy. This makes them more capable of spreading and more resistant to treatment. Fortunately, studies have shown that the consumption of an oxaloacetate supplement can decrease blood glutamate levels by 40%.[6,7] This leads to a reduction of tumor size and invasiveness.[8] Furthermore, patients who are given an oxaloacetate supplement experience an increased survival rate of 237%.[8]
Source with full text: CRONaxel Medical Food - Freeport Family Wellness Centre
Review Article | Published: 26 August 2016
Acetoacetate Assay Kit (Colorimetric) (ab180875) | Abcam
Acetoacetate (AcAc), a ß-ketoacid, is one of the three ketone bodies and is formed via condensation of two molecules of acetyl-CoA in liver mitochondria.
Conclusions
Our study suggests an important role of Glutamate oxaloacetate transaminase 1 (GOT1) to coordinate the glycolytic and the oxidative phosphorylation pathways in KRAS mutated cancer cells. GOT1 is crucial to provide oxaloacetate at low glucose levels, likely to maintain the redox homeostasis. Our data suggest GOT1 as a possible target in cancer therapy.
https://bmccancer.biomedcentral.com/articles/10.1186/s12885-018-4443-1
The metabolic fate of acetate in cancer
Abstract
Recent high-profile reports have reignited an interest in acetate metabolism in cancer. Acetyl-CoA synthetases that catalyse the conversion of acetate to acetyl-CoA have now been implicated in the growth of hepatocellular carcinoma, glioblastoma, breast cancer and prostate cancer. In this Review, we discuss how acetate functions as a nutritional source for tumours and as a regulator of cancer cell stress, and how preventing its (re)capture by cancer cells may provide an opportunity for therapeutic intervention.
Source: https://www.nature.com/articles/nrc.2016.87
Book source on cancer metabolism and oxaloacetate: Cancer
General information source: Is Cancer a Metabolic Disease? - ScienceDirect
Oxaloacetate is a new “Orphan Drug” for the treatment of Glioma
Study behind a paywall about CoA metabolism acetate and cancer: Acetate/acetyl-CoA metabolism associated with cancer fatty acid synthesis: Overview and application
Study: http://clincancerres.aacrjournals.o...rly/2015/03/26/1078-0432.CCR-14-1200.full.pdf
Acetate might be bad too in cancer:
The sources of acetyl-CoA and fatty acid synthesis
Acetyl-CoA is the precursor for the synthesis of fatty acids and cholesterol. Both glucose and glutamine can contribute to the generation of acetyl-CoA. Acetate has recently been shown to be yet another source of acetyl-CoA for many different cancer types, including breast, prostate, liver, primary glioblastomas and brain metastases. Some of these cancerous tissues incorporate acetate into fatty acids to support biomass production, whereas others have been shown to use acetate to fuel the TCA cycle (Comerford et al., 2014; Kamphorst et al., 2014; Mashimo et al., 2014; Schug et al., 2015). Mechanistically, acetate is ligated to CoA by the acyl-CoA synthetase short-chain family member 2 (ACSS2), an enzyme that is upregulated during conditions of metabolic stress such as low lipid availability and hypoxia. As such, acetate might become a crucial nutritional source in poorly vascularized regions of tumors.
Source: Cancer metabolism at a glance
Glyoxylic acid
Glyoxylic acid or oxoacetic acid is an organic compound. Together with acetic acid, glycolic acid, and oxalic acid, glyoxylic acid is one of the C2 carboxylic acids. It is a colourless solid that occurs naturally and is useful industrially.
"Historically glyoxylic acid was prepared from oxalic acid electrosynthetically:[7][8]
In organic synthesis, lead dioxide anodes were applied for the production of glyoxylic acid from oxalic acid in a sulfuric acid electrolyte.[9]
The conjugate base of glyoxylic acid is known as glyoxylate and is the form that the compound exists in solution at neutral pH. Glyoxylate is the byproduct of the amidation process in biosynthesis of several amidated peptides."
Source: Glyoxylic acid - Wikipedia
Glyoxylic... Hmm... Where have I heard that earlier... Glyoxylase?
CC: @Travis
Glycine does contain nitrogen but inhibits iNOS and lowers NO. Arginine seems to directly promote tumor growth. I think in advanced cancer cases where all ingested protein is quickly turned into ammonia, the best approach would be to supplement with keto-acids as they would combine with the high ammonia cancer patients have and help synthesize protein. Not sure if you have heard of Peat's famous "potato protein soup" but that is the rationale behind it.
Cancer patients overwhelmingly have negative nitrogen balance due to elevated cortisol, and administering steroids like T, DHT or synthetic AAS like oxandrolone has been shown to reverse that negative balance so if potato protein soup is not an option administering these steroids can reverse the catabolic state and allow regular protein to be eaten.
Some links on arginine and cancer.
Conditionally Essential Amino Acids: Glycine And Arginine
Arginine Depletion May Be A Viable Approach For Cancer
Glycine May Treat Lung, Brain And Other Cancers
https://www.cell.com/cell-reports/pdf/S2211-1247(16)31799-5.pdf
Keto acid - Wikipedia
Keto acids or ketoacids (also called oxo acids or oxoacids) are organic compounds that contain a carboxylic acid group and a ketone group.[1] In several cases, the keto group is hydrated. The alpha-keto acids are especially important in biology as they are involved in the Krebs citric acid cycle and in glycolysis.[2]
Common types of keto acids include:
- Alpha-keto acids, Alpha-ketoacids, or 2-oxoacids, such as pyruvic acid, have the keto group adjacent to the carboxylic acid. One important alpha-keto acid is oxaloacetic acid, a component of the Krebs cycle.[3] Another is alpha-ketoglutarate, is a 5-carbon ketoacid derived from glutamic acid. Alpha-ketoglutarate participates in cell signaling by functioning as a coenzyme,[4] and is commonly used in transamination reactions.
- Beta-keto acids, Beta-ketoacids, or 3-oxoacids, such as acetoacetic acid, have the ketone group at the second carbon from the carboxylic acid. They can be formed by the Claisen condensation.
- Gamma-keto acids, Gamma-ketoacids, or 4-oxoacids, such as levulinic acid, have the ketone group at the third carbon from the carboxylic acid.
When ingested sugars and carbohydrate levels are low, stored fats and proteins are the primary source of energy production. Glucogenic amino acids from proteins are converted to glucose. Ketogenic amino acids can be deaminated to produce alpha keto acids and ketone bodies.
Alpha keto acids are used primarily as energy for liver cells and in fatty acid synthesis, also in the liver.
Maybe either Oxaloacetic acid - Wikipedia or Acetoacetic acid - Wikipedia are good for cancer?
Acetoacetic acid (also diacetic acid) is the organic compound with the formula CH3COCH2COOH. It is the simplest beta-keto acid group, and like other members of this class, it is unstable. The methyl and ethyl esters, which are quite stable, are produced on a large scale industrially as precursors to dyes. Acetoacetic acid is a weak acid.[3]
Biochemistry
Under typical physiological conditions, acetoacetic acid exists as its conjugate base, acetoacetate.
Acetoacetate is produced in mitochondria of the liver from acetoacetyl Coenzyme A (CoA). First another acetyl group is added from acetyl CoA to form 3-hydroxy-3-methylgluteryl CoA, and then an acetyl CoA is lost from this yielding acetoacetate. The initial acetoacetate can come from the last cycle in the beta oxidation of a fatty acid, or it can be synthesized from two acetyl CoA molecules, catalyzed by thiolase.[4]
In mammals acetoacetate produced in the liver (along with the other two "ketone bodies") is released into the bloodstream as an energy source during periods of fasting, exercise, or as a result of type 1 diabetes mellitus.[5] First a CoA group is enzymatically transferred to it from succinyl CoA, converting it back to acetoacetyl CoA. This is then broken into two acetyl CoA molecules by thiolase, and these then enter the citric acid cycle. Heart muscle and renal cortex prefer acetoacetate over glucose. The brain uses acetoacetate when glucose levels are low due to fasting or diabetes.[6]
Acetoacetic acid - Wikipedia
Oxaloacetic acid (also known as oxalacetic acid) is a crystalline organic compound with the chemical formula HO2CC(O)CH2CO2H. Oxaloacetic acid, in the form of its conjugate base oxaloacetate, is a metabolic intermediate in many processes that occur in animals. It takes part in the gluconeogenesis, urea cycle, glyoxylate cycle, amino acid synthesis, fatty acid synthesis and citric acid cycle.[1]
Biosynthesis[edit]
Oxaloacetate forms in several ways in nature. A principal route is upon oxidation of L-malate, catalysed by malate dehydrogenase, in the citric acid cycle. Malate is also oxidized by succinate dehydrogenase in a slow reaction with the initial product being enol-oxaloacetate.[2]
It also arises from the condensation of pyruvate with carbonic acid, driven by the hydrolysis of ATP:
CH3C(O)CO2− + HCO3− + ATP → −O2CCH2C(O)CO2− + ADP + Pi
Occurring in the mesophyll of plants, this process proceeds via phosphoenolpyruvate, catalysed by pyruvate carboxylase.
Oxaloacetate can also arise from trans- or de- amination of aspartic acid.
Biochemical functions[edit]
Oxaloacetate is an intermediate of the citric acid cycle, where it reacts with acetyl-CoA to form citrate, catalysed by citrate synthase. It is also involved in gluconeogenesis, urea cycle, glyoxylate cycle, amino acid synthesis, and fatty acid synthesis. Oxaloacetate is also a potent inhibitor of Complex II.
Gluconeogenesis[edit]
Gluconeogenesis[1] is a metabolic pathway consisting of a series of eleven enzyme-catalyzed reactions, resulting in the generation of glucose from non-carbohydrates substrates. The beginning of this process takes place in the mitochondrial matrix, where pyruvate molecules are found. A pyruvate molecule is carboxylated by a pyruvate carboxylase enzyme, activated by a molecule each of ATP and water. This reaction results in the formation of oxaloacetate. NADH reduces oxaloacetate to malate. This transformation is needed to transport the molecule out of the mitochondria. Once in the cytosol, malate is oxidized to oxaloacetate again using NAD+. Then oxaloacetate remains in the cytosol, where the rest of reactions will take place. Oxaloacetate is later decarboxylated and phosphorylated by phosphoenolpyruvate carboxykinase and becomes 2-phosphoenolpyruvate using guanosine triphosphate (GTP) as phosphate source. Glucose is obtained after further downstream processing.
Urea cycle[edit]
The urea cycle is a metabolic pathway that results in the formation of urea using two ammonium molecules and one bicarbonate molecule.[1] This route commonly occurs in hepatocytes. The reactions related to the urea cycle produce NADH), and NADH can be produced in two different ways. One of these uses oxaloacetate. In the cytosol there are fumarate molecules. Fumarate can be transformed into malate by the actions of the enzyme fumarase. Malate is acted on by malate dehydrogenase to become oxaloacetate, producing a molecule of NADH. After that, oxaloacetate will be recycled to aspartate, as transaminases prefer these keto acids over the others. This recycling maintains the flow of nitrogen into the cell.
Glyoxylate cycle[edit]
The glyoxylate cycle is a variant of the citric acid cycle.[3] It is an anabolic pathway occurring in plants and bacteria utilizing the enzymes isocitrate lyase and malate synthase. Some intermediate steps of the cycle are slightly different from the citric acid cycle; nevertheless oxaloacetate has the same function in both processes.[1] This means that oxaloacetate in this cycle also acts as the primary reactant and final product. In fact the oxaloacetate is a net product of the glyoxylate cycle because its loop of the cycle incorporates two molecules of acetyl-CoA.
Fatty acid synthesis[edit]
In previous stages acetyl-CoA is transferred from the mitochondria to the cytoplasm where fatty acid synthase resides. The acetyl-CoA is transported as a citrate, which has been previously formed in the mitochondrial matrix from acetyl-coA and oxaloacetate. This reaction usually initiates the citric acid cycle, but when there is no need of energy it is transported to the cytoplasm where it is broken down to cytoplasmatic acetyl -CoA and oxaloacetate.
Another part of the cycle requires NADPH for the synthesis of fatty acids.[4] Part of this reducing power is generated when the cytosolic oxaloacetate is returned to the mitochondria as long as the internal mitochondrial layer is non-permeable for oxaloacetate. Firstly the oxaloacetate is reduced to malate using NADH. Then the malate is decarboxylated to pyruvate. Now this pyruvate can easily enter the mitochondria, where it is carboxylated again to oxaloacetate by pyruvate carboxylase. In this way, the transfer of acetyl-CoA that is from the mitochondria to the outside of the cell into the cytoplasm produces a molecule of NADH. The overall reaction, which is spontaneous, may be summarized as:
HCO3− + ATP + acetyl-CoA → ADP + Pi + malonyl-CoA
Amino acid synthesis[edit]
Six essential amino acids and three nonessential are synthesized from oxaloacetate and pyruvate.[5] Aspartate and alanine are formed from oxaloacetate and pyruvate, respectively, by transamination from glutamate. Asparagine, methionine, lysine and threonine are synthesized by aspartate, therefore given importance to oxaloacetate as without it, no aspartate would be formed and the following other amino acids would neither be produced.
Oxalate biosynthesis[edit]
Oxaloacetate produces oxalate by hydrolysis.[6]
oxaloacetate + H2O ⇌ oxalate + acetate
This process is catalyzed by the enzyme oxaloacetase.
Oxaloacetic acid - Wikipedia
Found this:
Acetoacetate is a metabolic inhibitor of cancer growth
Acetoacetate reduces growth and ATP concentration in cancer cell lines which over-express uncoupling protein 2. - PubMed - NCBI
Acetoacetate reduces growth and ATP concentration in cancer cell lines which over-express uncoupling protein 2
Addicted to AA (Acetoacetate): A Point of Convergence between Metabolism and BRAF Signaling
Prevention of Dietary-Fat-Fueled Ketogenesis Attenuates BRAF V600E Tumor Growth - ScienceDirect
Acetoacetate metabolism in AS-30D hepatoma cells
New Study Found Oxaloacetate Could Fight Cancer and Give Calorie Restriction Benefits
The metabolic fate of acetate in cancer
8) Oxaloacetate May Help Cancer
Glutamine is an important growth element for pancreatic cancer cells [R].
Studies have shown that reducing glutamine levels can stop cell growth of multiple forms of cancer [R].
Oxaloacetate has been shown to reduce glutamine levels and decrease cancer cell growth rates in mice [R].
It has also been shown to make chemotherapy and radiation treatment more effective [R].
Source: 15 Science-Based Health Benefits of Oxaloacetate - Selfhacked
Glutamine Addiction: A New Therapeutic Target in Cancer
Oxaloacetate induces apoptosis in HepG2 cells via inhibition of glycolysis
Oxaloacetate: 3 Outrageous Reasons This Molecule... - Nootropedia
Oxaloacetate: The Next Big Brain & Anti-Aging Supplement?
3 Ways an Oxaloacetate Supplement Can Protect You
CRONaxel is a US FDA registered combination of oxaloacetate and ascorbic acid for the clinical dietary management of the metabolic imbalances associated with certain cancers. (Oxaloacetate has the designation as an “orphan drug 12-3704” for the treatment of neuro-endocrine and glial tumors.)
Oxaloacetate is an obscure molecule that plays a role in energy production. Researchers have learned that it can also remove excess glutamate from the bloodstream. Glutamate can cause extensive brain damage in the event of a stroke or concussion, and it is a preferred fuel for many different types of cancer cells. Oxaloacetate’s removal of glutamate has a protective effect against these hazards.
Oxaloacetate increases energy production:
Cells can produce energy in two different ways. The more primitive, less effective method is glycolysis. The more advanced and efficient method is oxidative phosphorylation. This occurs in the mitochondria, and it produces eight times more energy than glycolysis—while using the same amount of fuel.[1] Oxaloacetate is an important part of the metabolic cycle that allows oxidative phosphorylation to occur. Without this molecule, cells are forced to rely more heavily on glycolysis.[2] This can lead to decreased production of energy and a decreased supply of blood sugar. In fact, studies indicate that a lack of oxaloacetate can cause energy production to fall by nearly 500%.[3]
Oxaloacetate starves cancer:
Cancerous cells rely on simple sugars and glutamate for their fuel supply, and this is especially true for brain tumors.[4] Glutamate also allows cancer cells to grow and divide.[5] When simple sugars and glutamate are abundant, cancer cells can produce more energy. This makes them more capable of spreading and more resistant to treatment. Fortunately, studies have shown that the consumption of an oxaloacetate supplement can decrease blood glutamate levels by 40%.[6,7] This leads to a reduction of tumor size and invasiveness.[8] Furthermore, patients who are given an oxaloacetate supplement experience an increased survival rate of 237%.[8]
Source with full text: CRONaxel Medical Food - Freeport Family Wellness Centre
Review Article | Published: 26 August 2016
Acetoacetate Assay Kit (Colorimetric) (ab180875) | Abcam
Acetoacetate (AcAc), a ß-ketoacid, is one of the three ketone bodies and is formed via condensation of two molecules of acetyl-CoA in liver mitochondria.
Conclusions
Our study suggests an important role of Glutamate oxaloacetate transaminase 1 (GOT1) to coordinate the glycolytic and the oxidative phosphorylation pathways in KRAS mutated cancer cells. GOT1 is crucial to provide oxaloacetate at low glucose levels, likely to maintain the redox homeostasis. Our data suggest GOT1 as a possible target in cancer therapy.
https://bmccancer.biomedcentral.com/articles/10.1186/s12885-018-4443-1
The metabolic fate of acetate in cancer
Abstract
Recent high-profile reports have reignited an interest in acetate metabolism in cancer. Acetyl-CoA synthetases that catalyse the conversion of acetate to acetyl-CoA have now been implicated in the growth of hepatocellular carcinoma, glioblastoma, breast cancer and prostate cancer. In this Review, we discuss how acetate functions as a nutritional source for tumours and as a regulator of cancer cell stress, and how preventing its (re)capture by cancer cells may provide an opportunity for therapeutic intervention.
Source: https://www.nature.com/articles/nrc.2016.87
Book source on cancer metabolism and oxaloacetate: Cancer
General information source: Is Cancer a Metabolic Disease? - ScienceDirect
Oxaloacetate is a new “Orphan Drug” for the treatment of Glioma
Study behind a paywall about CoA metabolism acetate and cancer: Acetate/acetyl-CoA metabolism associated with cancer fatty acid synthesis: Overview and application
Study: http://clincancerres.aacrjournals.o...rly/2015/03/26/1078-0432.CCR-14-1200.full.pdf
Acetate might be bad too in cancer:
The sources of acetyl-CoA and fatty acid synthesis
Acetyl-CoA is the precursor for the synthesis of fatty acids and cholesterol. Both glucose and glutamine can contribute to the generation of acetyl-CoA. Acetate has recently been shown to be yet another source of acetyl-CoA for many different cancer types, including breast, prostate, liver, primary glioblastomas and brain metastases. Some of these cancerous tissues incorporate acetate into fatty acids to support biomass production, whereas others have been shown to use acetate to fuel the TCA cycle (Comerford et al., 2014; Kamphorst et al., 2014; Mashimo et al., 2014; Schug et al., 2015). Mechanistically, acetate is ligated to CoA by the acyl-CoA synthetase short-chain family member 2 (ACSS2), an enzyme that is upregulated during conditions of metabolic stress such as low lipid availability and hypoxia. As such, acetate might become a crucial nutritional source in poorly vascularized regions of tumors.
Source: Cancer metabolism at a glance
Glyoxylic acid
Glyoxylic acid or oxoacetic acid is an organic compound. Together with acetic acid, glycolic acid, and oxalic acid, glyoxylic acid is one of the C2 carboxylic acids. It is a colourless solid that occurs naturally and is useful industrially.
"Historically glyoxylic acid was prepared from oxalic acid electrosynthetically:[7][8]
In organic synthesis, lead dioxide anodes were applied for the production of glyoxylic acid from oxalic acid in a sulfuric acid electrolyte.[9]
The conjugate base of glyoxylic acid is known as glyoxylate and is the form that the compound exists in solution at neutral pH. Glyoxylate is the byproduct of the amidation process in biosynthesis of several amidated peptides."
Source: Glyoxylic acid - Wikipedia
Glyoxylic... Hmm... Where have I heard that earlier... Glyoxylase?
I wonder how much of lactic acid produced is simply on account of the increased glyoxylase levels?
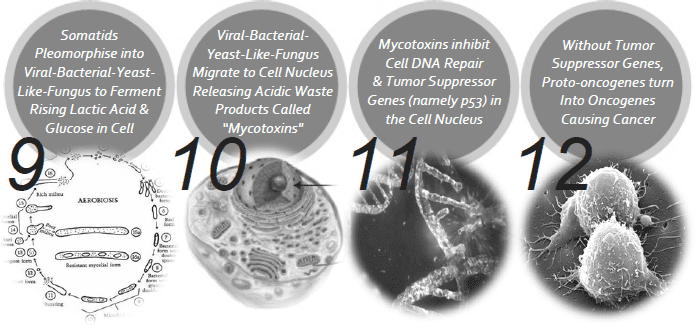
Glyoxylase I & II work in tandem to convert methylglyoxal into lactic acid, using glutathionine as a cofactor. Increased glyoxylase enzyme levels necessarily must lead to lower methylgloxal, lactic acid, and . . . perhaps even cancer:
Rulli, Antonio. "Expression of glyoxalase I and II in normal and breast cancer tissues." Breast cancer research and treatment (2001)
'A far higher activity level of glyoxylase I and II occurs in the tumor compared with pair-matched normal tissue, as shown by both spectrophotometrical assay and electrophoretic pattern. Such increased activities of glyoxylase I and II likely result from an enhanced enzyme synthesis as a consequence of increased expression of the respective genes in the tumoral tissue, as evidenced by northern blot.' ―Rulli
Paul Thornally is currently the leading authority on the methylglyoxal system, and has published many good articles on the topic. Doctor Thornally appears to have roughly 80 articles on methylglyoxal, but I do get the impression that he'd been given authorship credits in many of them simply on the basis of being advisor/editor of other peoples articles:
Thornalley, Paul J. "The glyoxalase system in health and disease." Molecular aspects of medicine (1993)
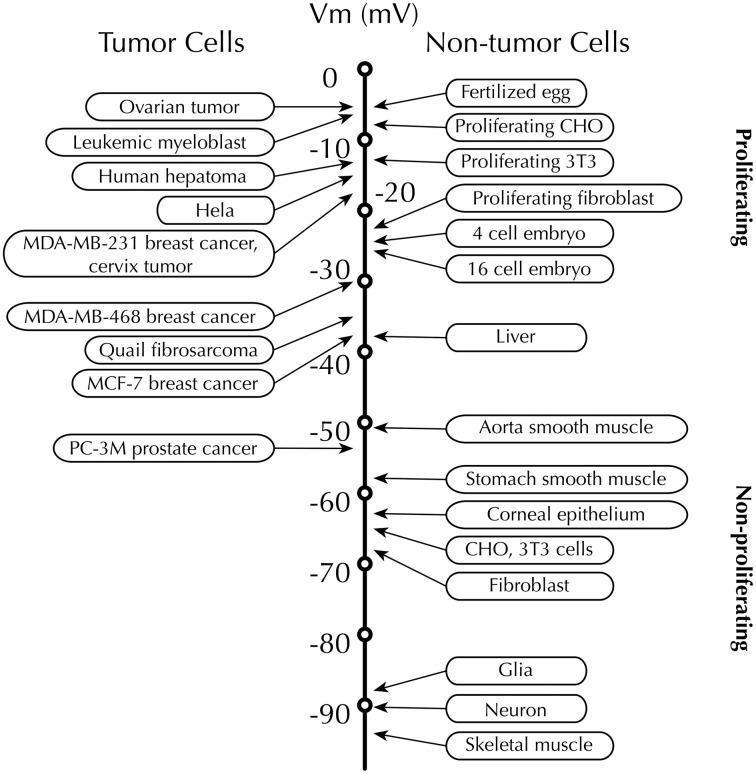
Other strong trends found in cancer cells are the increased expression of ornithine decarboxylase, increased stearoyl–CoA desaturase, and a diminished plasma membrane potential: Ornithine decarboxylase is of course the rate-limiting enzyme in polyamine synthesis, and polyamines physically bind dNA in a way that facilitates replication. Stearoyl–CoA desaturase tautologically desaturases stearate, when attached to coenzyme A, and increases membrane fluidity in this manner. For a cell to achieve one mitosis cycle, it needs to eventually double the amount of lipids on the cell membrane. You simply cannot achieve replication without the enzymes fatty acid synthase, stearoyl–CoA desaturase, and ornithine decarboxylase.
Lapachol and β-lapachone, found in pau d'arco, are two of the strongest glyoxylase inhibitors ever assayed. For inhibiting ornithine decarboxylase, thus decreasing polyamine synthesis, selenomethionine is a safe and natural amino acid to take—and one with other benefits besides: Some selenomethionine will eventually be metabolized, liberating inorganic selenium species that can be made available for selenocysteine synthesis. The enzyme glutathione peroxidase needs selenocysteine for reducing H₂O₂, and this enzyme can be synthesized using inorganic selenium (the inorganic selenium species is though to be added post-transcriptionally, meaning that ingesting selenocysteine proper is not required). By reducing cytosolic H₂O₂ concentrations, glutathione peroxidase lowers activation of NF-κB. This occurs because nuclear factor-κB is H₂O₂-sensitive, forming an internal disulfide bridge upon reacting with it. This achieves two ends: (1) it is then dissociated from its binding site, and (2) it is then compact enough to translocate into the cell's nucleus. The foregoing observations explain why inorganic selenium reduces cancer incidence, and also why selenomethionine—specifically—does that and more. [A person can also argue that it's the high methionine turnover of the prostate that accounts for selenomethionine's striking ability to reduce cancer there: the prostate synthesizes more polyamines than any other organ, and would of course need methionine to do so. This observation extends into the diagnostic realm, forming the basis for ¹¹C-methionine–PET imaging.]
CC: @Travis
Last edited: