Generous of your time to explain this, what doctors rarely know. Yeah just ask for a fasting insulin test and see what happens, or any discussion on insulemia or possible genetic factors...Hi Clash, thanks for post.
1. That is true, pure glucose causes the biggest spike in insulin response among a randomised group of people. However, within that same of randomised group of people, the peaks will look vastly different depending on their metabolic health profiles, which comes back to the original point, what causes metabolic disease, which in turn is the primary causal factor for hypertension, CVD, dementia, obesity, and all the other leading causes of deaths that I mentioned earler? Sucrose has a moderate glycemic index, but a substantially higher glycemic load, thanks to its fructose molecule that dilutes the pure glucose effect it has in these indicies when used for calculation, despite fructose, as opposed to fiber in most other foods as a component of total carbs, is just as bad if you were to build a metabolic index. The body appears to be excellently designed to handle a sudden rush of food, or glucose, with relative ease. However, repeated occurrences will eventually degrade that functionality.
2. Yes, as I had mentioned earlier, glucose causes the biggest increases in insulin response, but glucose is not found in pure form in nature, except through sucrose in the form of fiber rich fruits. It is very clear that amylose and amylopectins isocalorically given both lower peaks in insulin and lower AUC. These are crticial but not the only points needed to develop insulin resistance. Therefore, it is natural to conclude that pure sucrose is the easiest way to induce insulin resistance, not just for its readily absorbed glucose molecule, but also for its insulin independent fructose molecule.
3. That is not what the data show. It does not take extreme conditions to make the liver impaired, which I am assuming here your definition of that is oversupplied by energy and accumulated hepatic fat deposits through diet. In fact, you would be surprised to know that 30% of Americans have NAFLD, and up to 50% of the population in Korea, one of the remaining few countries that still uses HCFS (again, indistinguishable from sucrose as mentioned previously). It has been shown that countries that use HCFS as a sweetner had 20% more prevalence of diabetes, and much more for pre-diabetes, and this was adjusted for sugar intake, suggesting a calorie is not just a calorie. I would even go far as to say these figures are understating the problem. A 5% fractionation ja the official diagnosis of steatosis, I would love to see their serum hepatic lipase enzyme concentrations, using pre-diabetes to diabetes as an analogy, where the former is 80% of the problem, diabetes in itself is a small step towards disease compared to the more prevalent, more problematic, and less attention receiving hyperinsulinemia. So how would you make sure that DNL is at its highest? Simple, you consume sucrose, as also mentioned in a previous post, it works on two pathways independent of each of each other using glucose and fructose to create the ultimate DNL and cholesterol synthesis factory.
4. Good catch, I've been typing on my phone all this time which isn't the easiest thing to do.
5. Data points to that it does. This is especially evident in longitudinal studies, one of the key missing ingredients in most of the prospective or RCTs done. Much like ASCVD, It is a disease of progression.
6. I'm not very clear on your point. The pathopathology of type 1 and 2 diabetes is somewhat well understood, and sucrose consumption, especially in excess caloric surplus, is the primary driver of the latter.
7. They are not directly triggered by glucose or fructose ingestion, that is correct. They are triggered by the response of insulin which is normal and healthy, it is when insulin levels are both high and chronic, that issues arise. High levels of insulin, even in the presence of normal blood glucose levels as in pre-diabetics, I would argue make up 50% of the global population at minimum, can directly activate immune cells, particularly macrophages. Insulin can stimulate these cells to produce pro-inflammatory cytokines like TNF-alpha, IL-6, and IL-1β. Hyperinsulinemia can activate key signaling pathways within immune cells that sway kt towards a pro-inflammatory state. For example, the NF-κB pathway, a central regulator of inflammation, can be activated by high levels of insulin. This activation leads to the transcription of various genes involved in the inflammatory response. Insulin acts on the endothelium (the inner lining of blood vessels) and can influence the interaction between endothelial cells and immune cells. In a state of hyperinsulinemia, this interaction can become dysregulated, contributing to endothelial dysfunction and promoting the adhesion and migration of immune cells into tissues, thereby exacerbating inflammation. In conditions associated with hyperinsulinemia, such as obesity and metabolic syndrome, adipose tissue becomes inflamed and is characterized by an infiltration of immune cells. High insulin levels can exacerbate this inflammation in adipose tissue, leading to the release of more pro-inflammatory cytokines and adipokines. Chronic hyperinsulinemia can contribute to insulin resistance in immune cells themselves. This low-grade chronic inflammation is a hallmark of various metabolic disorders.
8. Sounds contradictory. You might want to re-read that one again, in the context of what I had said.
9. This is not true, given the data I have provided in this post and past posts. Pure fructose is not needed, and possibly inferior to sucrose in inducing non-subcutaneous adipose deposits.
10. To make it simple. Sucrose consumption, high insulin, fat liver deposits, liver insulin resistant, liver exports more glucose and TG which creates ROS, triggers immune response, immune cells insulin resistant and can neither utilise glucose or tell that glucose is now under control being in a perpetual inflammatory state, this is also partially done by reducing glucocorticoids that are anti-inflammatory in nature, cortisol eventually rises in insulin resistance as it fails to respond, cells become insulin resistant and glucocorticoid resistant, insulins mitogenic properties are still functional leading to stiffening of artierial walls and endothelial dysfunction raising blood pressure, liver exporting much higher lipoprotein particles due to increased DNL and inhibited glucogenesis get pushed against the damaged endothelial wall more readily and get stuck, more immune response, plaque formation and CVD. It is a vicious self feeding cycle.
Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
-
By using this site you agree to the terms, rules, and privacy policy.
-
Charlie's Restoration Giveaway #2 (Entire Home EMF Mitigation & Protection Along With Personal Protection) - Click Here To Enter
-
Dear Carnivore Dieters, A Muscle Meat Only Diet is Extremely Healing Because it is a Low "vitamin A" Diet. This is Why it Works so Well...
Rest the rest of this post by clicking here
-
The Forum is transitioning to a subscription-based membership model - Click Here To Read
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Sucrose is the primary source of modern disease
- Thread starter Alpha
- Start date
Alpha
Member
- Joined
- Nov 16, 2018
- Messages
- 236
My definition of pre-diabetic is different than most people. It's hyperinsulinemia with normal blood glucose. Fasting insulin levels doesn't show you hyperinsulinemia. The insulin responses are sometimes higher in "normal" patients than in type-2 diabetes, but they clear faster so you will never see it fasting. Some doctors are starting to catch up and doing TG, LDL and BG tests few hours after eating, these are the most relevant levels.Generous of your time to explain this, what doctors rarely know. Yeah just ask for a fasting insulin test and see what happens, or any discussion on insulemia or possible genetic factors...
If you look 2h-post prandial stimulated insulin there was no difference between 5%, 6%, 7%, 8%, and 9% Hb1Ac, because it measures glycation of blood glucose over time, and stops being sensitive over around 5.0-5.5%. For context, the cutoff for prediabetes is 5.7%, and for diabetes its 6.5%. In fact, the very disease Hb1Ac is supposed to measure, which is type 2 diabetes, it has a sensitivity of about 55% for an 80% specificity because it was designed that way. It's better to delay the diagnosis of diabetes than falsely tell a patient he has diabetes when he doesn't, this is word-for-word coming from the ADA.
I would look for 5 biomarkers to identify metabolic dysfunction:
1- Blood pressure over 120/80
2- Abdomen fat
3- Hepatic lipase
4- Uric acid
5- Post-prandial insulin and TG
I think you are spot on.My definition of pre-diabetic is different than most people. It's hyperinsulinemia with normal blood glucose. Fasting insulin levels doesn't show you hyperinsulinemia. The insulin responses are sometimes higher in "normal" patients than in type-2 diabetes, but they clear faster so you will never see it fasting. Some doctors are starting to catch up and doing TG, LDL and BG tests few hours after eating, these are the most relevant levels.
If you look 2h-post prandial stimulated insulin there was no difference between 5%, 6%, 7%, 8%, and 9% Hb1Ac, because it measures glycation of blood glucose over time, and stops being sensitive over around 5.0-5.5%. For context, the cutoff for prediabetes is 5.7%, and for diabetes its 6.5%. In fact, the very disease Hb1Ac is supposed to measure, which is type 2 diabetes, it has a sensitivity of about 55% for an 80% specificity because it was designed that way. It's better to delay the diagnosis of diabetes than falsely tell a patient he has diabetes when he doesn't, this is word-for-word coming from the ADA.
I would look for 5 biomarkers to identify metabolic dysfunction:
1- Blood pressure over 120/80
2- Abdomen fat
3- Hepatic lipase
4- Uric acid
5- Post-prandial insulin and TG
At my local needlepushing medic, fasting insulin (upon insistence) is observed once then once 2hrs after. Sigh.
Alpha
Member
- Joined
- Nov 16, 2018
- Messages
- 236
I have not seen that study. If that were true, the results further add to the detrimental effects of fructose, because it is telling you that fructose increases gram-negative bacterial lipopolysaccarihdes in the gut. By blocking TLR4, you are not fixing the problem, you are suppressing your body's immune response to pathogens which will ultimatley make the problem worse.there was a study where they took mice and knocked out the TLR4 receptor, making them immune to endotoxin in a sense. These researchers found these knockout TLR4 micedid not develop fatty liver or insulin ressitance from fructose, while the normal mice did. Wouldn't that mean that endotoxin is to blame and not fructose per se?
Liver steatosis and insulin resistance is also inhibited in SCB1 -/- mice, the primary gene for carbohydrate and dietary fat metabolism. It does that mostly through transcription of SREBP-1c. Fructose, much more strongly than glucose, activates that pathway.
Fructose-only diet compared to chow resulted in 2.6x more SREBP-1c, 19.6x SCD-1, 7.0x more Fatty Acid synthase, and 9.1x ACC enzyme.
Oleic acid combined with Fructose also showed to be worse through SCD-1 independent pathways on FAS and ACC
SREBP-1c -/- did not have an impact, suggesting it is mostly done through SCD1. The data on fructose and in turn sucrose is overwhelmingly clear. That northern blotting should stop anyone from consuming sucrose if you understand what it means.
Last edited:
Yeah but the fact that rats who had the tlr4 receptor knocked out didn't suffer at all kind of allocates the problem entirely to endotoxin in a way.I have not seen that study. If that were true, the results further add to the detrimental effects of fructose, because it is telling you that fructose increases gram-negative bacterial lipopolysaccarihdes in the gut. By blocking TLR4, you are not fixing the problem, you are suppressing your body's immune response to pathogens which will ultimatley make the problem worse.
Liver steatosis and insulin resistance is also inhibited in SCB1 -/- mice, the primary gene for carbohydrate and dietary fat metabolism. It does that mostly through transcription of SREBP-1c. Fructose, much more strongly than glucose, activates that pathway.
View attachment 59772
Fructose-only diet compared to chow resulted in 2.6x more SREBP-1c, 19.6x SCD-1, 7.0x more Fatty Acid synthase, and 9.1x ACC enzyme.
View attachment 59773
Oleic acid combined with Fructose also showed to be worse through SCD-1 independent pathways on FAS and ACC
View attachment 59774
SREBP-1c -/- did not have an impact, suggesting it is mostly done through SCD1. The data on fructose and in turn sucrose is overwhelmingly clear. That northern blotting should stop anyone from consuming sucrose if you understand what it means.
View attachment 59775
I'm very surprised that you're still focusing on fructose on this endotoxin issue, there are many reason for why someone can have gut problems and eating something like fructose could just show the damage to an already damaged system.
Gut motility is common reason for bad gut issues. I do not believe there is good or bad bacteria, there are enough horror stories of people taking probiotics with sibo to convince me on this.
I think it's more so related to slow gut motility, which can be caused from many different things.
A mixed diet for one can slow gastric emptying because of the huge amounts of fat in the diet, which I need to mention that these rat studies with tlr4 were studied on a diet of high fructose AND high fat in both arms of the study.
This gives a good reason for why fructose would increase endotoxin in these rats. The fat was slowing down the gut motility and this the bacteria had time to feed on the fructose and increase the endotoxin load in the gut.
Alpha
Member
- Joined
- Nov 16, 2018
- Messages
- 236
Yeah but the fact that rats who had the tlr4 receptor knocked out didn't suffer at all kind of allocates the problem entirely to endotoxin in a way.
I'm very surprised that you're still focusing on fructose on this endotoxin issue, there are many reason for why someone can have gut problems and eating something like fructose could just show the damage to an already damaged system.
Gut motility is common reason for bad gut issues. I do not believe there is good or bad bacteria, there are enough horror stories of people taking probiotics with sibo to convince me on this.
I think it's more so related to slow gut motility, which can be caused from many different things.
A mixed diet for one can slow gastric emptying because of the huge amounts of fat in the diet, which I need to mention that these rat studies with tlr4 were studied on a diet of high fructose AND high fat in both arms of the study.
This gives a good reason for why fructose would increase endotoxin in these rats. The fat was slowing down the gut motility and this the bacteria had time to feed on the fructose and increase the endotoxin load in the gut.
If you have been reading all of this threading thus far, you wouldn't be asking those questions. Microbiota that leans towards pathological have to do primarily with lack fiber and SCFA/MCFA, and secondly the inflammation from sucrose and fructose consumption. If you consume pure sucrose or fructose, they get absorbed way up in the gut, they never reach mid to lower intestines or the colon where the majority of your gut microbiota are. Yet, it causes overgrowth of bad bacteria in those areas where no food is reached. Why is that? Because Fructose doesn't show the damage, fructose is the damage.
Background/Aims
Consumption of refined carbohydrates in soft drinks has been postulated to be a key factor in the development of non-alcoholic fatty liver disease (NAFLD). The aim of the present study was to test the effects of ad libitum access to different sugars consumed in drinking water on hepatic fat accumulation.
Methods
For 8 weeks, C57BL/J6 mice had free access to solutions containing 30% glucose, fructose, sucrose, or water sweetened with artificial sweetener (AS) or plain water. Body weight, caloric intake, hepatic steatosis and lipid peroxidation were assessed.
Results
Total caloric intake and weight gain were highest in mice exposed to glucose. In contrast, hepatic lipid accumulation was significantly higher in mice consuming fructose compared to all other groups. Moreover, endotoxin levels in portal blood and lipid peroxidation as well as TNFα expression were significantly higher in fructose fed mice than in all other groups. Concomitant treatment of fructose fed mice with antibiotics (e.g., polymyxin B and neomycin) markedly reduced hepatic lipid accumulation in fructose fed mice.
Conclusions
These data support the hypothesis that high fructose consumption may not only lead to liver damage through overfeeding but also may be directly pro-inflammatory by increasing intestinal translocation of endotoxin.
I'll leave you with this study to go through, instead of me dissecting each one.
Taken together, our data further support the hypothesis that a diet rich in fructose may at least in part add to the onset of NAFLD through mechanisms involving an increased translocation of intestinal microbial components, altered concentration of TLR and activation of TLR-dependent signalling pathways. Our data further suggest that fructose may alter intestinal permeability through altering tight junction proteins (e.g. occludin) in the duodenum directly rather than altering intestinal microbiota composition.
Toll-like receptors 1–9 are elevated in livers with fructose-induced hepatic steatosis | British Journal of Nutrition | Cambridge Core
Toll-like receptors 1–9 are elevated in livers with fructose-induced hepatic steatosis - Volume 107 Issue 12
Before I answer all of this, I would like to ask where you draw the line in terms of foods with sucrose in them being healthy or unhealthy. For example, fruit.If you have been reading all of this threading thus far, you wouldn't be asking those questions. Microbiota that leans towards pathological have to do primarily with lack fiber and SCFA/MCFA, and secondly the inflammation from sucrose and fructose consumption. If you consume pure sucrose or fructose, they get absorbed way up in the gut, they never reach mid to lower intestines or the colon where the majority of your gut microbiota are. Yet, it causes overgrowth of bad bacteria in those areas where no food is reached. Why is that? Because Fructose doesn't show the damage, fructose is the damage.
Background/Aims
Consumption of refined carbohydrates in soft drinks has been postulated to be a key factor in the development of non-alcoholic fatty liver disease (NAFLD). The aim of the present study was to test the effects of ad libitum access to different sugars consumed in drinking water on hepatic fat accumulation.
Methods
For 8 weeks, C57BL/J6 mice had free access to solutions containing 30% glucose, fructose, sucrose, or water sweetened with artificial sweetener (AS) or plain water. Body weight, caloric intake, hepatic steatosis and lipid peroxidation were assessed.
Results
Total caloric intake and weight gain were highest in mice exposed to glucose. In contrast, hepatic lipid accumulation was significantly higher in mice consuming fructose compared to all other groups. Moreover, endotoxin levels in portal blood and lipid peroxidation as well as TNFα expression were significantly higher in fructose fed mice than in all other groups. Concomitant treatment of fructose fed mice with antibiotics (e.g., polymyxin B and neomycin) markedly reduced hepatic lipid accumulation in fructose fed mice.
Conclusions
These data support the hypothesis that high fructose consumption may not only lead to liver damage through overfeeding but also may be directly pro-inflammatory by increasing intestinal translocation of endotoxin.
I'll leave you with this study to go through, instead of me dissecting each one.
View attachment 59784
View attachment 59785
Toll-like receptors 1–9 are elevated in livers with fructose-induced hepatic steatosis | British Journal of Nutrition | Cambridge Core
Toll-like receptors 1–9 are elevated in livers with fructose-induced hepatic steatosis - Volume 107 Issue 12www.cambridge.org
ATP
Member
- Joined
- Oct 15, 2015
- Messages
- 279
If you have been reading all of this threading thus far, you wouldn't be asking those questions. Microbiota that leans towards pathological have to do primarily with lack fiber and SCFA/MCFA, and secondly the inflammation from sucrose and fructose consumption. If you consume pure sucrose or fructose, they get absorbed way up in the gut, they never reach mid to lower intestines or the colon where the majority of your gut microbiota are. Yet, it causes overgrowth of bad bacteria in those areas where no food is reached. Why is that? Because Fructose doesn't show the damage, fructose is the damage.
Background/Aims
Consumption of refined carbohydrates in soft drinks has been postulated to be a key factor in the development of non-alcoholic fatty liver disease (NAFLD). The aim of the present study was to test the effects of ad libitum access to different sugars consumed in drinking water on hepatic fat accumulation.
Methods
For 8 weeks, C57BL/J6 mice had free access to solutions containing 30% glucose, fructose, sucrose, or water sweetened with artificial sweetener (AS) or plain water. Body weight, caloric intake, hepatic steatosis and lipid peroxidation were assessed.
Results
Total caloric intake and weight gain were highest in mice exposed to glucose. In contrast, hepatic lipid accumulation was significantly higher in mice consuming fructose compared to all other groups. Moreover, endotoxin levels in portal blood and lipid peroxidation as well as TNFα expression were significantly higher in fructose fed mice than in all other groups. Concomitant treatment of fructose fed mice with antibiotics (e.g., polymyxin B and neomycin) markedly reduced hepatic lipid accumulation in fructose fed mice.
Conclusions
These data support the hypothesis that high fructose consumption may not only lead to liver damage through overfeeding but also may be directly pro-inflammatory by increasing intestinal translocation of endotoxin.
I'll leave you with this study to go through, instead of me dissecting each one.
View attachment 59784
View attachment 59785
Toll-like receptors 1–9 are elevated in livers with fructose-induced hepatic steatosis | British Journal of Nutrition | Cambridge Core
Toll-like receptors 1–9 are elevated in livers with fructose-induced hepatic steatosis - Volume 107 Issue 12www.cambridge.org
fructose is the damage.
It's crazy you're still on the Peat forum trying to argue that sugar consumption is the MAIN CAUSE of disease. There are plenty of places where you will find like minded people that share your sentiment.
I'll leave you with this study to go through, instead of me dissecting each one.
Where are the human studies (RCTs, MA) showing sucrose is the main cause of disease in a cohort that are consuming glucose + fructose compared to those who aren't with energy equivalent diets?
Fructose is a burden on the liver, glucose is not. Toxicity is the primary source of modern disease. Fructose allow those toxins to accumulate due to being a burden. Glucose is fuel for the liver to detox, glucose is the way.
Low vitamin A fruits like apples and bananas are safe unless the person is severely compromised then those would want to be limited until they are more robust.
Low vitamin A fruits like apples and bananas are safe unless the person is severely compromised then those would want to be limited until they are more robust.
Alpha
Member
- Joined
- Nov 16, 2018
- Messages
- 236
Well that depends. How much alcohol do you think is a healthy amount to take a day? Fructose is alcohol in the body. They are identical. How do we used to get alcohol? Fermenting fruits.Before I answer all of this, I would like to ask where you draw the line in terms of foods with sucrose in them being healthy or unhealthy. For example, fruit.
It used to be the popular belief for a long time that 1 drink a day or a few drinks a week was heart healthy and pro-aging. There was seemingly a J-curve effect where if you ingested more alcohol than that, it started being detrimental. Well it was recently discovered that there is no amount of alcohol that is healthy. Just like fructose, that number is zero. But why did there used to be a difference? Well turns out, the beneficial effects of reservatrol on SIRT-1 was stronger than a small amount of alcohol that the liver can generally handle, generally leaving to the same or better outcomes than no alcohol. It was also found that there was a correlation between people who drank a few times a week socially were of higher socio-economic status, more sociable, and had a higher quality of life, and better emotional health, all things that confounded with a longer healthier life span.
A comprehensive insight into the potential effects of resveratrol supplementation on SIRT-1: A systematic review - PubMed
The results of the included studies showed that resveratrol supplementation had beneficial effects on protein and gene expression of SIRT1.
Until recently, fruits were only consumed seasonally, that was evident in our evolutionary past, and you can still see that in great apes, or hunter-gatherer tribes still alive today. The reason for that is fruits are hibernation food, the storgae of metabolically active adipose tissue around the liver and organs help go through periods of low food reserves and cold temperatures. They effectively slowed down metabolism to conserve energy, and will sometimes be associated with a longer life, particularly through SIRT-2, the same effect is achieved through caloric restriction, in a sirtuin dependent pathway. Fruit production also used to be controlled by annual rainfall, which differed from year to year. Humans and primates have a self-regulating feedback in the brain where if you consume sugar in the form of fruits after the first few, depending on current hormone profile and energy reserves, will taste much less sweet and shift preference to vegetables, insects, or other types of food. That does not exist with white sugar where fiber is lacking and the amount of sugar present in a single bite or drink is too large to kick in that mechanism early enough before overconsumption.
Fruits have a significantly high number of polyphenols and anti-oxidants that are very beneficial and generally protect against the negative effects of sucrose, the fiber will also allow a portion of that fructose not to be fully absorbed in the gut, and maintaining gut lining integrity in the process.
For an unhealthy person cosuming lifelong sugars, I would say no amount of fruit is good until they return to health, then having fruits as part of the diet is viable, in moderation.
Taken together, all evidence show there is no healthy amount of sucrose consumption outside of fruits and whole foods, and likely fruit consumption should be taken with caution in individuals with metabolic dysfunction until optimal health is achieved.
Last edited:
mayku-T-meelo
Member
- Joined
- Sep 24, 2016
- Messages
- 188
So in essence, you are blaming fructose?
Since you've invested a lot of time in dissecting this topic on your own and this thread being an anti-Peat thread, I'm interested, how do you examine Peat's view on it? How do you comment on Peat's understanding of fructose being the beneficial part of sucrose? What are the false assumptions of his reasoning? In short, he states that fructose is basically helping with absorbing and utilizing glucose, lowers the need for insulin and aids thermogenesis.
"Many people lately have been told, as part of a campaign to explain the high incidence of fatty liver degeneration in the US, supposedly resulting from eating too much sugar, that fructose can be metabolized only by the liver. The liver does have the highest capacity for metabolizing fructose, but the other organs do metabolize it."
"Besides being one of the forms of sugar involved in ordinary energy production, interchangeable with glucose, fructose has some special functions, that aren't as well performed by glucose. It is the main sugar involved in reproduction, in the seminal fluid and intrauterine fluid, and in the developing fetus. After these crucial stages of life are past, glucose becomes the primary molecular source of energy, except when the system is under stress. It has been suggested (Jauniaux, et al., 2005) that the predominance of fructose rather than glucose in the embryo's environment helps to maintain ATP and the oxidative state (cellular redox potential) during development in the low-oxygen environment. The placenta turns glucose from the mother's blood into fructose, and the fructose in the mother's blood can pass through into the fetus, and although glucose can move back from the fetus into the mother's blood, fructose is unable to move in that direction, so a high concentration is maintained in the fluids around the fetus."
"Besides protecting against the reductive stresses, fructose can also protect against the oxidative stress of increased hydrogen peroxide (Spasojevic, et al., 2009). Its metabolite, fructose 1,6-bisphosphate, is even more effective as an antioxidant."
"Many stressors cause capillary leakage, allowing albumin and other blood components to enter extracellular spaces or to be lost in the urine, and this is a feature of diabetes, obesity, and a variety of inflammatory and degenerative diseases including Alzheimer's disease (Szekanecz and Koch, 2008; Ujiie, et al., 2003). Although the mechanism isn't understood, fructose supports capillary integrity; fructose feeding for 4 and 8 weeks caused a 56% and 51% reduction in capillary leakage, respectively (Chakir, et al., 1998; Plante, et al., 2003)."
"Lipid peroxidation is involved in the degenerative diseases, and many publications argue that fructose increases it, despite the fact that it can increase the production of uric acid, which is a major component of our endogenous antioxidant system (e.g., Waring, et al., 2003). When rats were fed for 8 weeks on a diet with 18% fructose and 11% saturated fatty acids, the content of polyunsatured fats in the blood decreased, as they had in the Brown, et al., experiment, and their total antioxidant status was increased (Girard, et al., 2005). When stroke-prone spontaneously hypertensive rats were given 60% fructose, superoxide dismutase in their liver was increased, and the authors suggest that this "may constitute an early protective mechanism" (Brosnan and Carkner, 2008). When people were given a 300 calorie drink containing glucose, or fructose, or orange juice, those receiving the glucose had a large increase in oxidative and inflammatory stress (reactive oxygen species, and NF-kappaB binding), and those changes were absent in those receiving the fructose or orange juice (Ghanim, et al., 2007)."
from newsletter Sugar Issues
Since you've invested a lot of time in dissecting this topic on your own and this thread being an anti-Peat thread, I'm interested, how do you examine Peat's view on it? How do you comment on Peat's understanding of fructose being the beneficial part of sucrose? What are the false assumptions of his reasoning? In short, he states that fructose is basically helping with absorbing and utilizing glucose, lowers the need for insulin and aids thermogenesis.
"Many people lately have been told, as part of a campaign to explain the high incidence of fatty liver degeneration in the US, supposedly resulting from eating too much sugar, that fructose can be metabolized only by the liver. The liver does have the highest capacity for metabolizing fructose, but the other organs do metabolize it."
"Besides being one of the forms of sugar involved in ordinary energy production, interchangeable with glucose, fructose has some special functions, that aren't as well performed by glucose. It is the main sugar involved in reproduction, in the seminal fluid and intrauterine fluid, and in the developing fetus. After these crucial stages of life are past, glucose becomes the primary molecular source of energy, except when the system is under stress. It has been suggested (Jauniaux, et al., 2005) that the predominance of fructose rather than glucose in the embryo's environment helps to maintain ATP and the oxidative state (cellular redox potential) during development in the low-oxygen environment. The placenta turns glucose from the mother's blood into fructose, and the fructose in the mother's blood can pass through into the fetus, and although glucose can move back from the fetus into the mother's blood, fructose is unable to move in that direction, so a high concentration is maintained in the fluids around the fetus."
"Besides protecting against the reductive stresses, fructose can also protect against the oxidative stress of increased hydrogen peroxide (Spasojevic, et al., 2009). Its metabolite, fructose 1,6-bisphosphate, is even more effective as an antioxidant."
"Many stressors cause capillary leakage, allowing albumin and other blood components to enter extracellular spaces or to be lost in the urine, and this is a feature of diabetes, obesity, and a variety of inflammatory and degenerative diseases including Alzheimer's disease (Szekanecz and Koch, 2008; Ujiie, et al., 2003). Although the mechanism isn't understood, fructose supports capillary integrity; fructose feeding for 4 and 8 weeks caused a 56% and 51% reduction in capillary leakage, respectively (Chakir, et al., 1998; Plante, et al., 2003)."
"Lipid peroxidation is involved in the degenerative diseases, and many publications argue that fructose increases it, despite the fact that it can increase the production of uric acid, which is a major component of our endogenous antioxidant system (e.g., Waring, et al., 2003). When rats were fed for 8 weeks on a diet with 18% fructose and 11% saturated fatty acids, the content of polyunsatured fats in the blood decreased, as they had in the Brown, et al., experiment, and their total antioxidant status was increased (Girard, et al., 2005). When stroke-prone spontaneously hypertensive rats were given 60% fructose, superoxide dismutase in their liver was increased, and the authors suggest that this "may constitute an early protective mechanism" (Brosnan and Carkner, 2008). When people were given a 300 calorie drink containing glucose, or fructose, or orange juice, those receiving the glucose had a large increase in oxidative and inflammatory stress (reactive oxygen species, and NF-kappaB binding), and those changes were absent in those receiving the fructose or orange juice (Ghanim, et al., 2007)."
from newsletter Sugar Issues
@Alpha
Hi,
What elements or experiences make you think that fructose and alcohol are the same thing?
In my expérience, i eat "fructose rich foods", i very rarely drink alcohol, the majority of "fructose rich foods" have 0 alcohol taste, and the effects are totally different from alcohol, there are slight negative effects that I can feel even with half a sip of alcohol, whereas I can eat kilos of "fructose rich fruits/foods" without feeling these negative effects,
The only very rare time I've eaten a honey that had a distinguishable slight taste of alcohol, I've felt the slight negative effects that I feel even from half a sip of alcoholic drinks
99.999% "fructose rich foods" had neither the taste nor the effects of alcohol
Hi,
What elements or experiences make you think that fructose and alcohol are the same thing?
In my expérience, i eat "fructose rich foods", i very rarely drink alcohol, the majority of "fructose rich foods" have 0 alcohol taste, and the effects are totally different from alcohol, there are slight negative effects that I can feel even with half a sip of alcohol, whereas I can eat kilos of "fructose rich fruits/foods" without feeling these negative effects,
The only very rare time I've eaten a honey that had a distinguishable slight taste of alcohol, I've felt the slight negative effects that I feel even from half a sip of alcoholic drinks
99.999% "fructose rich foods" had neither the taste nor the effects of alcohol
Last edited:
I would just like to say that when I was on the carnivore diet for 6 months, I started dreaming of fruit and craving it badly, I didn't for one second crave starch, maybe buttered potatoes on occasion. But it was mainly fruit.Well that depends. How much alcohol do you think is a healthy amount to take a day? Fructose is alcohol in the body. They are identical. How do we used to get alcohol? Fermenting fruits.
It used to be the popular belief for a long time that 1 drink a day or a few drinks a week was heart healthy and pro-aging. There was seemingly a J-curve effect where if you ingested more alcohol than that, it started being detrimental. Well it was recently discovered that there is no amount of alcohol that is healthy. Just like fructose, that number is zero. But why did there used to be a difference? Well turns out, the beneficial effects of reservatrol on SIRT-1 was stronger than a small amount of alcohol that the liver can generally handle, generally leaving to the same or better outcomes than no alcohol. It was also found that there was a correlation between people who drank a few times a week socially were of higher socio-economic status, more sociable, and had a higher quality of life, and better emotional health, all things that confounded with a longer healthier life span.
A comprehensive insight into the potential effects of resveratrol supplementation on SIRT-1: A systematic review - PubMed
The results of the included studies showed that resveratrol supplementation had beneficial effects on protein and gene expression of SIRT1.pubmed.ncbi.nlm.nih.gov
Until recently, fruits were only consumed seasonally, that was evident in our evolutionary past, and you can still see that in great apes, or hunter-gatherer tribes still alive today. The reason for that is fruits are hibernation food, the storgae of metabolically active adipose tissue around the liver and organs help go through periods of low food reserves and cold temperatures. They effectively slowed down metabolism to conserve energy, and will sometimes be associated with a longer life, particularly through SIRT-2, the same effect is achieved through caloric restriction, in a sirtuin dependent pathway. Fruit production also used to be controlled by annual rainfall, which differed from year to year. Humans and primates have a self-regulating feedback in the brain where if you consume sugar in the form of fruits after the first few, depending on current hormone profile and energy reserves, will taste much less sweet and shift preference to vegetables, insects, or other types of food. That does not exist with white sugar where fiber is lacking and the amount of sugar present in a single bite or drink is too large to kick in that mechanism early enough before overconsumption.
Fruits have a significantly high number of polyphenols and anti-oxidants that are very beneficial and generally protect against the negative effects of sucrose, the fiber will also allow a portion of that fructose not to be fully absorbed in the gut, and maintaining gut lining integrity in the process.
For an unhealthy person cosuming lifelong sugars, I would say no amount of fruit is good until they return to health, then having fruits as part of the diet is viable, in moderation.
Taken together, all evidence show there is no healthy amount of sucrose consumption outside of fruits and whole foods, and likely fruit consumption should be taken with caution in individuals with metabolic dysfunction until optimal health is achieved.
Sugar seems to be more beneficial from a hormonal point of view where it lowers cortisol better than starch, I think in some instances starch can actually raise cortisol due to it's hypoglycemic effects.
I have a major problem with the way you are tackling fructose. What's very interesting is I used to think sugar was really bad, but I did keto and carnivore for 1.5 years and although I looked healthy, I felt absolutely terrible.
I experimented with mostly starch (mashed potatoes, white rice, oat bran)as my carb after those diets, I gained alot of weight eating that way. I also felt terrible, no energy, feeling very irritable and just very depressed.
When I switched to mostly fruit as my carb source, i leaned out, lost alot of fat not sure if I gained muscle or not, but I look good i think.
Throughout the entirety of reintroducing carbohydrates into my diet I have been dealing with severe gut issues, namely bloating, gas and slow gut motility. It was particularly bad while eating alot of fruit juices and just very refined sources of sucrose.
The starch phase did help my digestive issues to an extent, but it made me feel awful and just not very nice to be around. I felt very depressed while on starch.
Switching from starch to fruit was incredible, my bowel motility seemed to speed up, my gut issues seemed to not get any worse and my skin also started to clear up more.
As of now I'm still dealing with issues, but I've noticed that if I put my digestive health first and consume foods to help with that, then o start to feel much better.
Is it the fructose that's a burden on the liver, or the endotoxin that it creates from bacterial fermentation?Fructose is a burden on the liver, glucose is not. Toxicity is the primary source of modern disease. Fructose allow those toxins to accumulate due to being a burden. Glucose is fuel for the liver to detox, glucose is the way.
Low vitamin A fruits like apples and bananas are safe unless the person is severely compromised then those would want to be limited until they are more robust.
Alpha
Member
- Joined
- Nov 16, 2018
- Messages
- 236
Hi Truth.@Alpha
Hi,
What elements or experiences make you think that fructose and alcohol are the same thing?
In my expérience, i eat "fructose rich foods", i very rarely drink alcohol, the majority of "fructose rich foods" have 0 alcohol taste, and the effects are totally different from alcohol, there are slight negative effects that I can feel even with half a sip of alcohol, whereas I can eat kilos of "fructose rich fruits/foods" without feeling these negative effects,
The only very rare time I've eaten a honey that had a distinguishable slight taste of alcohol, I've felt the slight negative effects that I feel even from half a sip of alcoholic drinks
99.999% "fructose rich foods" had neither the taste nor the effects of alcohol
The processing of fructose in the liver is not controlled by hormone or allosteric mechanisms, and fructose bypasses the rate-limiting step of glycolysis catalyzed by phosphofructokinase 1 (PFK 1). Hence, fructose metabolism is less tightly regulated and occurs at a much faster rate than glucose. The same story with alcohol, ethanol enters the hepatocyte through osmosis, it does not require insulin for its metabolism, and it does not stimulate insulin secretion. Both molecules have metabolites that activate the SREBP-1c which is essential for activating triglyceride synthesis and inhibiting oxidation, like I mentioned earlier.
Although the absolute rate of DNL of ethanol (i.e., that which is metabolized to VLDL) is relatively small, fractional DNL increases from 1% at baseline to 31% after an ethanol bolus. Similarly, there was a study in humans that showed more than 4 servings of fruit a day increased fat mass, insulin resistance, and liver steatosis, a finding that has been overwhelmingly consistent among alcohol and fructose.
Here is a paper that shows you the similarities between ethanol and fructose on metabolism and enzymatic pathways.
More importantly as I have mentioned before, when the liver receives glucose and fructose simultaneously as is in the case of sucrose, there is a synergistic pathway where the glucose occupies the glycogenic pathway, forcing the fructose down the lipogenic pathway, thus tripling the rate of DNL compared with just fructose alone. This is also clear with consumption of ethanol in combination with either glucose, fructose, or both.
The oxidation of ethanol is irreversible and unregulated just like fructose in the liver, making the rate dependent only on local concentration and enzyme activity. This unregulated reduction lowers cytoplasmic and mitochondrial NAD+ and, through the latter, cellular energy in ATP/AMP ratio goes down. Importantly, decreased AMP through a lower rate of ATP synthesis decreases AMP-dependent protein kinase (AMPK) activity, an important regulator of cellular energy metabolism. The depletion of NAD+ does two things, one, it chronically suppresses AMPK and the sitruins associated with metabolic health, and two it disrupts oxidative phosphorylation forcing the pyruvate pathway outside the mitochondria towards lactate, positioning the organism through lactic acidosis.
If you have read anything I've written thus far, it is virtually identical to the process by which fructose disrupts metabolic health. As far as the liver is concerned, the only organ that can absorb and metabolize both, they are indistinguishable metabolically, and of course the dose makes the posion, a shot of spiri alcohol would have around 20g of ethanol, a similar amount of fructose would need 2 Hershey's milk chocolate bar.
De novo lipogenesis, lipid kinetics, and whole-body lipid balances in humans after acute alcohol consumption - PubMed
We conclude that the consumption of 24 g alcohol activates the hepatic DNL pathway modestly, but acetate produced in the liver and released into plasma inhibits lipolysis, alters tissue fuel selection, and represents the major quantitative fate of ingested ethanol.
De novo lipogenesis, lipid kinetics, and whole-body lipid balances in humans after acute alcohol consumption - PubMed
We conclude that the consumption of 24 g alcohol activates the hepatic DNL pathway modestly, but acetate produced in the liver and released into plasma inhibits lipolysis, alters tissue fuel selection, and represents the major quantitative fate of ingested ethanol.
Fructose: It’s “Alcohol Without the Buzz”
What do the Atkins Diet and the traditional Japanese diet have in common? The Atkins Diet is low in carbohydrate and usually high in fat; the Japanese diet is high in carbohydrate and usually low in fat. Yet both work to promote weight loss. One commonality ...
A Dual Sugar Challenge Test for Lipogenic Sensitivity to Dietary Fructose
An oral challenge of glucose and fructose gives a robust lipogenic response as measured from the increase in VLDL triglyceride palmitate over 4 hours.Increased hepatic de novo lipogenesis (DNL) in response to dietary sugar is implicated in dyslipidemia, ...
Hello,
Without quoting specific papers or studies unless requested, it's been very obvious to me that sucrose, which is one part glucose, one part fructose, is the main source of metabolic syndrome, which in turn is the umbrella condition that leads to the other more commonly known diseases such as Atherosclerosis Cardiovascular Disease (ASCVD), Dementia, Diabates, Obesity, Stroke, and Renal disease. These diseases contribute to 25% of worldwide annual deaths, which for all intent and purposes, are almost entirely preventable. I have not included cancer, which is about 15% of total deaths on its own, to sugar given the highly complex and number of pathophysiologies involved to attribute it to one single factor, although I am happy to entertain the idea that it can be significantly reduced, or alternatively is highly predictable through sucrose consumption.
Table sugar, or added sugars are the main component of total sugars consumed by the average person in their diet, although high fructose corn syrup (HFCS), although banned or scarce in most of the developed world, is still being used widely in the US or East Asia, also falls under that category since they are essentially metabolically equivalent in the human body.
This is a thread to discuss and post resources regarding the most convincing, or the latest scientific research regarding sucrose, or fructose consumption.
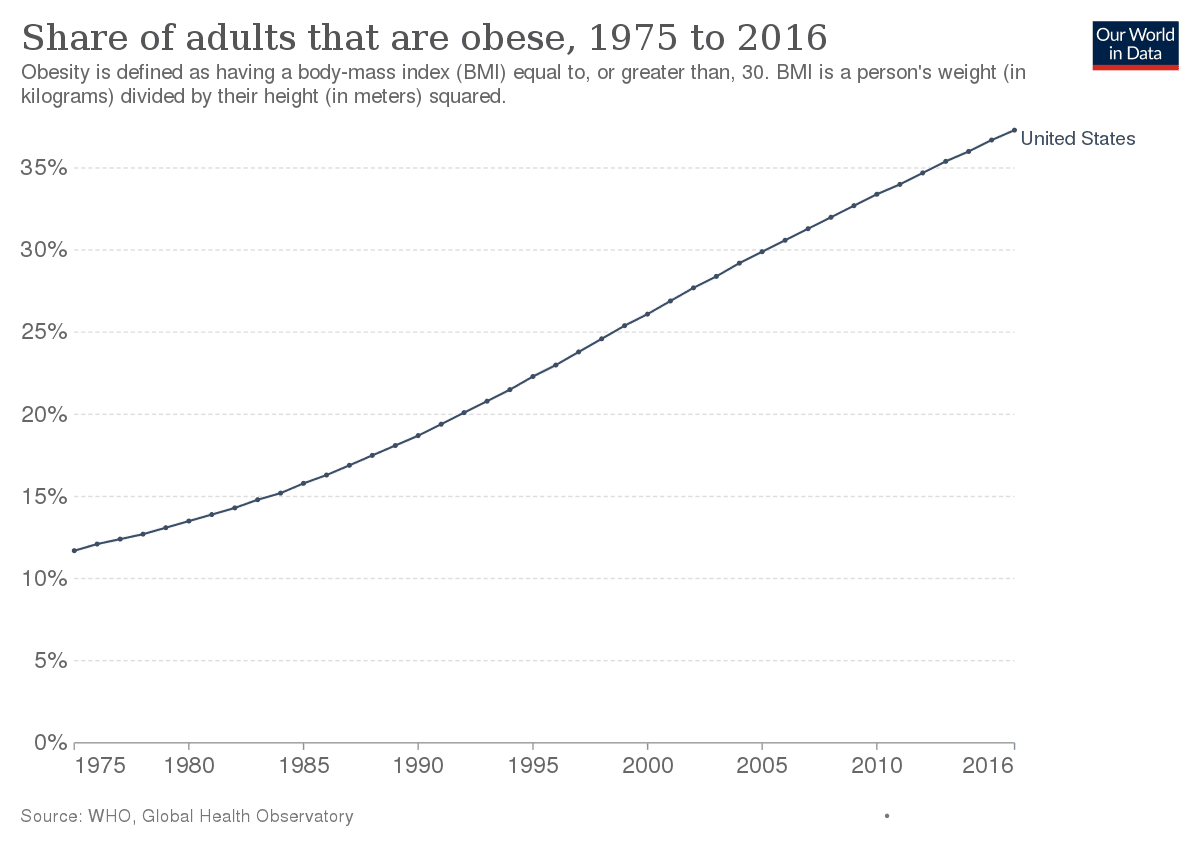
Not true. Sugar ("refined cane and beet sugar" in the graph below) consumption has been steadily decreasing since the 1970s and is currently at its lowest level ever, while obesity rates have skyrocketed since the 1970s and have not had even a single year or flattening/reversal.
The Dose Makes the Poison: Sugar and Obesity in the United States – a Review
Two-thirds of the US population is either overweight or obese. Obesity is one of the major drivers of preventable diseases and health care costs. In the US, current estimates for these costs range from $147 to $210 billion per year. Obesity is a multifactorial ...
In fact, even if you look at total carb (sugar + other types) consumption. the rate per capita in the US is at the levels of 1970-1980s (see above link), and in 1975 the obesity rate was 10%-12% while now it is ~40% (see below).
Obesity in the United States - Wikipedia
So, sucrose consumption and obesity rates would be very strongly negatively correlated if one were to use those curves shown in the graphs above. Furthermore, if you look at rates for cancer, CVD, dementia, Parkinson, etc you will see that those have also been rising since 1975 and overlap almost perfectly with the rise in obesity rates, and inversely correlated with sugar consumption. Worse, the mortality from the major chronic diseases has also been rising since the 1970s and shows no sign of abating.
The Top 3 Causes of Diabetes | The Motley Fool
Affecting more than 25 million people in the U.S., here are the primary factors that lead to this potentially debilitating disease and what's being done to curb its growth.
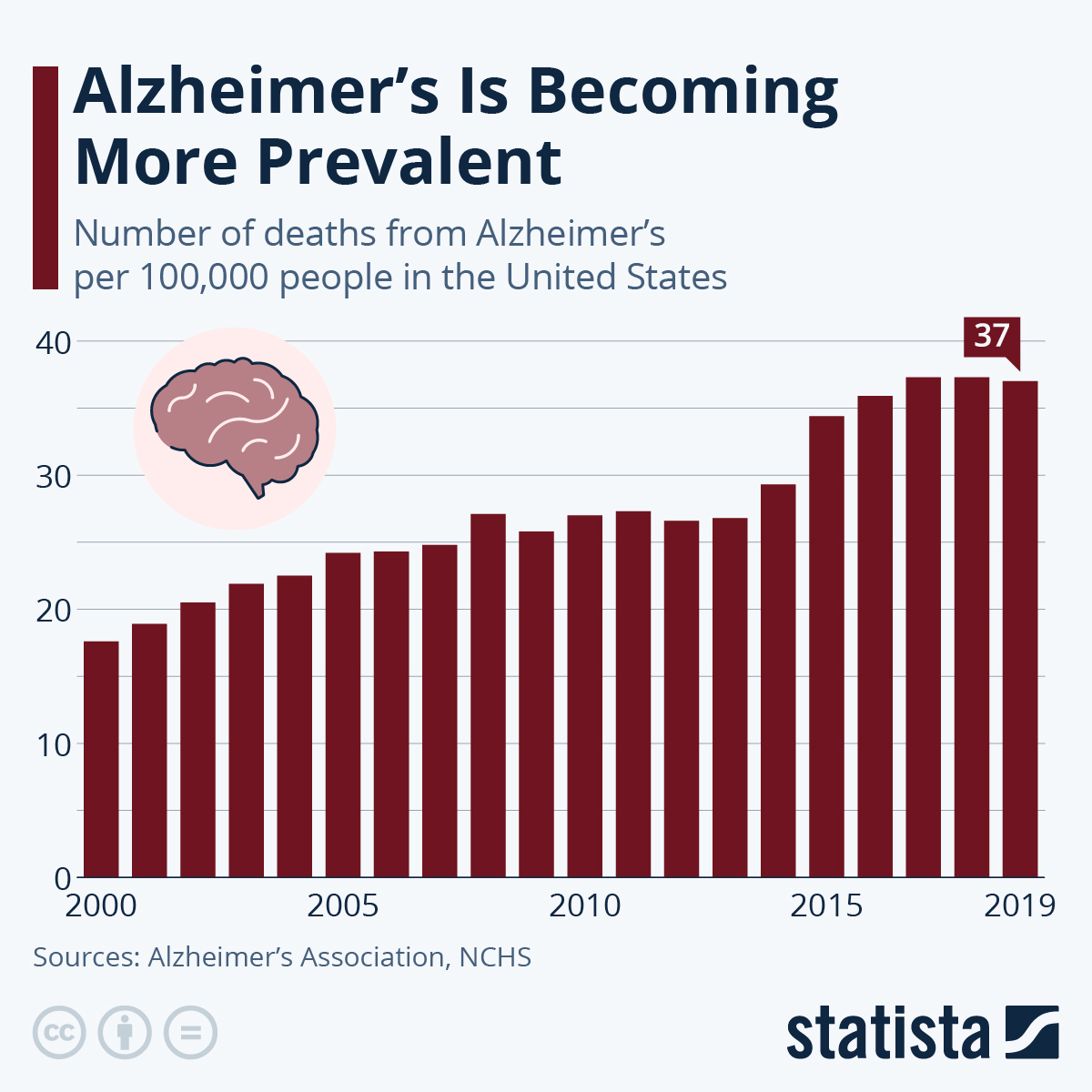
Infographic: Alzheimer’s Is Becoming More Prevalent
This chart shows the number of deaths from Alzheimer's disease per 100,000 people in the United States between 2000 and 2019.
@Peatful
Last edited:
Mauritio
Member
- Joined
- Feb 26, 2018
- Messages
- 5,669
The biggest part of fructose does not even reach the liver, but its metabolized by the gut.Hi Truth.
The processing of fructose in the liver is not controlled by hormone or allosteric mechanisms, and fructose bypasses the rate-limiting step of glycolysis catalyzed by phosphofructokinase 1 (PFK 1). Hence, fructose metabolism is less tightly regulated and occurs at a much faster rate than glucose. The same story with alcohol, ethanol enters the hepatocyte through osmosis, it does not require insulin for its metabolism, and it does not stimulate insulin secretion. Both molecules have metabolites that activate the SREBP-1c which is essential for activating triglyceride synthesis and inhibiting oxidation, like I mentioned earlier.
Although the absolute rate of DNL of ethanol (i.e., that which is metabolized to VLDL) is relatively small, fractional DNL increases from 1% at baseline to 31% after an ethanol bolus. Similarly, there was a study in humans that showed more than 4 servings of fruit a day increased fat mass, insulin resistance, and liver steatosis, a finding that has been overwhelmingly consistent among alcohol and fructose.
Here is a paper that shows you the similarities between ethanol and fructose on metabolism and enzymatic pathways.
View attachment 59810
View attachment 59811
More importantly as I have mentioned before, when the liver receives glucose and fructose simultaneously as is in the case of sucrose, there is a synergistic pathway where the glucose occupies the glycogenic pathway, forcing the fructose down the lipogenic pathway, thus tripling the rate of DNL compared with just fructose alone. This is also clear with consumption of ethanol in combination with either glucose, fructose, or both.
The oxidation of ethanol is irreversible and unregulated just like fructose in the liver, making the rate dependent only on local concentration and enzyme activity. This unregulated reduction lowers cytoplasmic and mitochondrial NAD+ and, through the latter, cellular energy in ATP/AMP ratio goes down. Importantly, decreased AMP through a lower rate of ATP synthesis decreases AMP-dependent protein kinase (AMPK) activity, an important regulator of cellular energy metabolism. The depletion of NAD+ does two things, one, it chronically suppresses AMPK and the sitruins associated with metabolic health, and two it disrupts oxidative phosphorylation forcing the pyruvate pathway outside the mitochondria towards lactate, positioning the organism through lactic acidosis.
If you have read anything I've written thus far, it is virtually identical to the process by which fructose disrupts metabolic health. As far as the liver is concerned, the only organ that can absorb and metabolize both, they are indistinguishable metabolically, and of course the dose makes the posion, a shot of spiri alcohol would have around 20g of ethanol, a similar amount of fructose would need 2 Hershey's milk chocolate bar.
View attachment 59812
View attachment 59813
De novo lipogenesis, lipid kinetics, and whole-body lipid balances in humans after acute alcohol consumption - PubMed
We conclude that the consumption of 24 g alcohol activates the hepatic DNL pathway modestly, but acetate produced in the liver and released into plasma inhibits lipolysis, alters tissue fuel selection, and represents the major quantitative fate of ingested ethanol.pubmed.ncbi.nlm.nih.gov
De novo lipogenesis, lipid kinetics, and whole-body lipid balances in humans after acute alcohol consumption - PubMed
We conclude that the consumption of 24 g alcohol activates the hepatic DNL pathway modestly, but acetate produced in the liver and released into plasma inhibits lipolysis, alters tissue fuel selection, and represents the major quantitative fate of ingested ethanol.pubmed.ncbi.nlm.nih.gov
Fructose: It’s “Alcohol Without the Buzz”
What do the Atkins Diet and the traditional Japanese diet have in common? The Atkins Diet is low in carbohydrate and usually high in fat; the Japanese diet is high in carbohydrate and usually low in fat. Yet both work to promote weight loss. One commonality ...www.ncbi.nlm.nih.gov
A Dual Sugar Challenge Test for Lipogenic Sensitivity to Dietary Fructose
An oral challenge of glucose and fructose gives a robust lipogenic response as measured from the increase in VLDL triglyceride palmitate over 4 hours.Increased hepatic de novo lipogenesis (DNL) in response to dietary sugar is implicated in dyslipidemia, ...www.ncbi.nlm.nih.gov
- Fructose Is NOT Metabolized By The Liver But The Small Intestines
Fructose does not cause fatty liver unless bacteria (--> endotoxin--> serotonin) are present.
- Lack of liver steatosis in germ-free mice following hypercaloric diets, serotonin causative
So it is more of a gut /microbiome than a liver or fructose issue.
DNL is almost negligible even with overfeeding people basic table sugar:
sphenoid
Member
- Joined
- Jul 17, 2021
- Messages
- 60
Wouldn’t the presence of GLUT5 also greatly influence fructose metabolism? Impaired metabolism/low thyroid/stress will result in reduced expression of the protein causing fructose to be absorbed poorly, allowing for fermentation and subsequent endotoxin formation.
EMF Mitigation - Flush Niacin - Big 5 Minerals
Similar threads
- Replies
- 1
- Views
- 4K
- Replies
- 61
- Views
- 13K
- Replies
- 3
- Views
- 3K
- Replies
- 5
- Views
- 3K
- Replies
- 6
- Views
- 3K
- Replies
- 5
- Views
- 4K
- Replies
- 9
- Views
- 4K
- Replies
- 52
- Views
- 15K
- Replies
- 3
- Views
- 2K
- Replies
- 100
- Views
- 40K
